The Importance of Improving Identification and Care of GBV Survivors
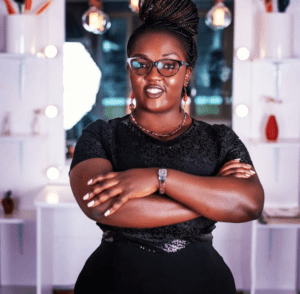
By Luseka Mwanzi, Gender Coordinator
Gender-based violence (GBV) has rapidly gained attention around the world over the past 50 years with international and local efforts in place to prevent GBV and support survivors. However, amidst COVID-19 lockdowns, there has been a disturbing increase in GBV with many survivors unable to leave their homes.
Improving identification and care of GBV survivors is critical as it enables health care providers to provide an accurate diagnosis and offer the most appropriate care, while ensuring the survivor is getting the critical care they need. Many conditions, such as chronic pain, repeat cases of violence, or reoccurring sexually-transmitted infections, can be difficult to diagnose or treat without knowing about a person’s experience of violence. Therefore, staff who fail to consider the possibility that women, men, or children are living in violent circumstances may not successfully identify a GBV survivor.
During the COVID-19 lockdown, we have provided virtual and tele-support to health facilities to improve identification, care, and treatment of GBV survivors. By using real facility-level data provided by the health care workers and training facilities on WI-HER’s iDARE methodology, WI-HER, through the USAID Afya Nyota ya Bonde Project in Kenya, supported facilities to develop their own unique goals, identify barriers to achieving those goals, and test solutions to achieve each goal. We supported facilities and used existing national and international tools to support their work, including applying the World Health Organization’s LIVES (listen, inquire, validate, enhance, and support) for first line support.
With a gender equity and social inclusion (GESI) approach in place for the purpose of improving identification and care of GBV survivors, facilities were able to identify men as victims of violence. Prior to the training male GBV survivors of all ages were rarely identified and often missed; therefore, they were not provided with the care they needed, which can contribute to a cycle of violence.
Through the first line support, survivors are also made aware of other available services of referral such as legal services and shelter services, among others. This is possible because, through improved identification and care of GBV survivors, there is better coordination and referrals within and between hospital departments as well as other departments, such as the legal and social services departments.
Improved identification and care of GBV survivors enables survivors to feel comfortable in speaking about their experiences, because it is done in a private setting and confidentiality is ensured. For a very long time, GBV has been an issue that has been looked at with a lot of stigma by society; providing an environment where survivors feel free and safe is very important in post-GBV clinical care.
Although a lot needs to be done to prevent GBV in homes and communities, the COVID-19 pandemic has made this incredibly challenging. In the meantime, we will continue to support health workers in identifying GBV survivors at the facility or in the community, and providing quality care, including psychosocial support.